
A guide on TAPVR and TA.
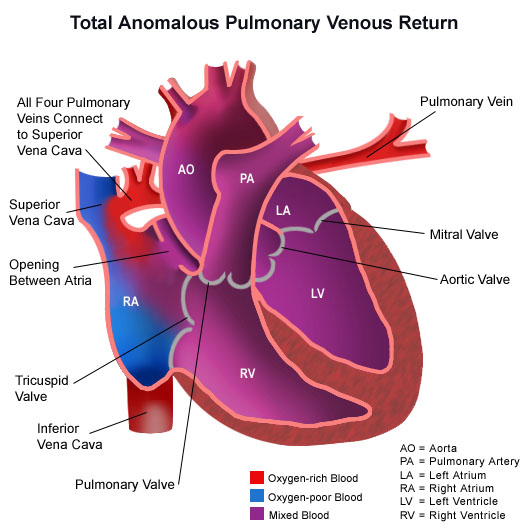
TOTAL ANOMALOUS PULMONARY VENOUS RETURN
What is TAPVR?
TAPVR is also known as Total Anomalous Pulmonary Venous Return. It is a congenital defect described as the pulmonary veins of the heart are misplaced.
Pulmonary veins, which take blood from the lungs should be normally connected in the left atrium. In TAPVR, these pulmonary veins are found in the different part of the heart.
INCIDENCE
It accumulates 2% of all congenital heart disorders.
Occurs approximately 4-6 in 100,000 live births.
CAUSES
Generally, CHDs causes are unknown. IT may be because of the following factors:
genes or chromosomes
environmental factors
medications
PATHOPHYSIOLOGY





SIGNS and SYMPTOMS
Right atrial enlargement
Right ventricular hypertrophy
Pulmonary hypertension
Mild cyanosis
Pulmonary edema
DIAGNOSTIC TESTS
Chest X -Ray - to indentify pulmonary edema
EKG - to locate right venticular hypertrophy
Echocardiogram - locates ASD, enlargement of right atrium and right ventricular hypertophy

medical mgt
Obstructed total anomalous pulmonary venous connection (TAPVC) presents immediately after birth with severe cyanosis and poor systemic perfusion and constitutes a medical and surgical emergency.
Sedation, ventilation, or hyperventilation with 100% oxygen - to improve effective pulmonary blood flow.
Administration of prostaglandin E1 (eg, alprostadil, PGE1) - increase systemic cardiac output
correction of systemic acidosis with sodium bicarbonate - to improve oxygen-delivery capacity.
In neonates or infants with unobstructed TAPVC, medical therapy is directed at compensating right ventricular failure, hypoxia, and congestive heart failure.

SURGICAL MGT
Balloon atrial septostomy (BAS) is done to decompress the venous circuit and improve cardiac output in cases of a restrictive inter-atrial communication.
10-15% of patients undergoing repair of TAPVC require multiple interventions due to recurrent stenosis after initial successful correction, with an increasingly poor outcome at each representation.
TRUNCUS ARTERIOSUS
WHAT IS TRUNCUS ARTERIOSUS?
Truncus Arteriosus or also known as TA, is a congenital heart disease that is described as one major artery or "trunk" arises from the left and right ventricle.
Oxygen poor blood that should go to the lungs and oxygen rich blood that should go to the rest of the body are mixed together.
INCIDENCE
A very RARE disorder.
Accumulates 1% of initial cardiac lesions.
Causes
CHD's generally have unknown causes.
Some of the risk factors are:
viral illness during early pregnancy
poorly controlled diabetes
certain meds
chromosomal disorder
smoking
PATHOPHYSIOLOGY
first few days of life
SIGNS and SYMPTOMS
Cyanosis
poor feeding
pounding heart
irritability
lethargy
poor growth
dyspnea
tachypnea
clubbing
MANAGEMENT

Medical

surgical
MEDICAL MGT
Digitalis and diuretic medicines for CHF
Intravenous prostaglandin to correct duct-dependent systemic or pulmonary blood flow
Afterload reducing agents, inotropic medications, or antiarrhythmics.
Full-term and premature newborns with truncus arteriosus may be at increased risk for necrotizing enterocolitis, either preoperatively or postoperatively, and appropriate evaluation should be undertaken in any newborn exhibiting signs or symptoms of necrotizing enterocolitis.
SURGICAL MGT
Truncus arteriosus invariably requires operative repair as early as possible.
Currently, surgical management consists of:
Complete primary repair, with closure of the ventricular septal defect, committing the common arterial trunk to the left ventricle, and reconstruction of the right ventricular outflow tract.
In patients with one pulmonary artery arising from the common trunk and one from the underside of the aortic arch, the pulmonary arteries are disconnected separately; they are then anastomosed together before being anastomosed to the conduit or are anastomosed to the conduit independently.
The following nursing diagnosis, prevention and discharge planning are BOTH for TAPVR and TA.
Decreased cardiac output r/t cardiac malformations
Observation of the quality and strength of heart rate, peripheral pulses, skin color and warmth.
Enforce the degree of cyanosis (circumoral, mucous membranes, clubbing).
Monitor signs of CHF (restlessness, tachycardia, tachypnea, tightness, fatigue, periorbital edema, oliguria, and hepatomegaly).
Collaboration of digoxin appropriate order, using the toxicity hazard prevention techniques.
Give treatment to reduce afterload.
Give diuretics as indicated.


Impaired Gas Exchange r/t to Pulmonary Congestion
Monitor the quality and respiratory rhythm.
Adjust the position of the child with Fowler position.
Avoid child of an infected person.
Give adequate rest.
Provide optimal nutrition.
Give oxygen if indicated.

Activity Intolerance r/t Cardiac Malformations
Allow the child to rest frequently, and avoid disturbances during sleep.
Encourage games and activities to do lightly.
Help the child to choose activities appropriate to the age, condition and ability of the child.
Avoid the ambient temperature is too hot or too cold.
Avoid the things that cause fear / anxiety in children.
Altered Growth and Development r/t Inadequate Oxygen and Nutrients
Provide a balanced diet, high nutrients to achieve adequate growth.
Monitor height and weight, documented in the form of graphs to identify trends in the growth of the child.
Measure body weight each day with the same weight and the same time.
Record intake and output correctly.
Give food with small portions but often to avoid fatigue at meals.
Children who receive diuretics are usually very thirsty, therefore not restricted fluid.
Risk for Infection r/t Decrease in Health Status
Avoid contact with infected individuals.
Give adequate rest.
Give the optimal nutritional needs.
Ensure optimal environment

PREVENTION
THERE IS NO DEFINITE WAY TO PREVENT BOTH DISEASES BUT YOU CAN ALWAYS REDUCE THE RISK FACTORS TO AVOID IT.

References
https://www.cdc.gov/ncbddd/heartdefects/tapvr.html
https://medlineplus.gov/ency/article/001115.htm
https://www.slideshare.net/pawandeep8/total-anomalous-pulmonary-venous-connections-seminar-ppt
http://emedicine.medscape.com/article/902981-treatment#d14
https://www.cincinnatichildrens.org/health/t/tapvr